This week, the 2015 HIMSS Patient Engagement Summit is taking place in sunny, warm Orlando. According to HIMMS, conference attendees will learn how “leading healthcare organizations” are successfully using health IT and other strategies to engage patients in their care.
Patient  What I suspect attendees will not hear much about at the Summit (particularly from speakers and exhibitors – one in the same?) is the growing “disillusionment” with the ability of patient portals, EHRs/PHRs and smart apps to actually engage patients at all. One only need look at the dismal adoption rates of these technologies (in the very low double digits if that) within most provider organizations, Kaiser, Group Health and Geisinger being notable exceptions.
What I suspect attendees will not hear much about at the Summit (particularly from speakers and exhibitors – one in the same?) is the growing “disillusionment” with the ability of patient portals, EHRs/PHRs and smart apps to actually engage patients at all. One only need look at the dismal adoption rates of these technologies (in the very low double digits if that) within most provider organizations, Kaiser, Group Health and Geisinger being notable exceptions.
What disillusionment you may ask?
Recently I conducted my own informal poll on LinkedIn’s HIMSS Group by ask the following question:
If a patient chose NOT to use your patient portal, PHR or smart health apps do you consider them to be “unengaged” in their own healthcare?
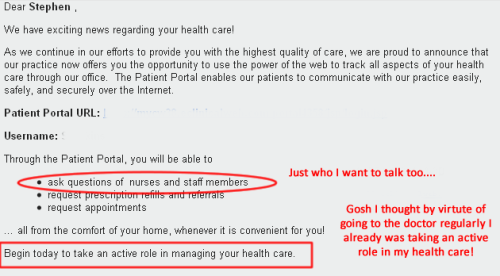
The question was prompted by all the “over the top claims” by HIMSS (See their Patient Engagement Framework) and EHR and Health IT bloggers that patient portals, EHRs and smart apps are what drive patient engagement. Come on now.
If that were true, that would mean that prior to the World Wide Web in the early 1990’s it was impossible for people to be engaged in their own healthcare. That is simply not true!
Who doesn’t recall Healthwise’s big old health handbook. It must have weighed 5lbs! Or who doesn’t remember “Ask A Nurse” – that ubiquitous 1-800 number you could call at 3:00 AM a health question? And of course there was always the doctor, family member or friend you could discuss your health concern with. To this day, more health conversations among seniors probably occur in McDonalds over morning coffee than on some EMR or health app.
But I digress…
So what were the results of my informal poll?
Take a look for yourself. Below are snippets from some of the 70+ responses (and counting) I received from members of the HIMSS Group which consists of developers, venture capitalists, informatics, vendors and clinicians.
What surprised me the most was how few “good things” people had to say about health IT in general…not just with regards to patient engagement.
- I am in healthcare IT and I still have not used my EPIC portal for scheduling an appt, view results, etc. because it is has been too much trouble to access.
- Are they “unengaged” if they do not use these tools? Absolutely not. [ . . .] I actually consider patients who use the portal, PHR or apps and are NOT having direct contact face-to-face or by telehealth as being “unengaged”. Patient engagement is a very personal and individual decisions made by the patient and can change drastically at any given time.
- It seems we too often try to use technology to replace human interaction. Patient engagement requires human interaction and collaborative work between the provider and patient.
- Until the portal becomes a) easy to use and relevant, b) doesn’t have 20 pages of legalese and c) can converse with you via email, txt, Instant Messages or phone; there will always be a substantial portion of the population that won’t use them.
- Ok, [patient portals]not normally a big deal until you read the terms of service which, paraphrasing the legalese, said “If we are breached, it is your fault. We are not responsible for losses you might incur. If it is determined that the entire system was compromised through your account you will be responsible for our costs to remedy the situation”.
- Match […]the technology to the message. I am aware of HIPAA secure phone mail systems that get 83% of patients using the system to listen to messages left for them by a clinician within 24 hours. We are all used to voice mail and using the phone.
- Engagement should be defined by the level of interaction with a provider, and the resulting outcomes. So, no, I think assessing level of engagement by use of the technology is pretty limited.
- If you want to know why patients and physicians do not use portals, it is because they are designed by EHR companies that design them as poorly as they design EHRs. Combine that with Byzantine security procedures, and you get a somewhat useless system.
- The assumption that a percent of users accessing data on a portal = patient engagement is where we fail! A percentage of people will access a portal for various reasons, and they will also NOT access a portal for various reasons. The real question should be…. what can we do to make the info easier to access and easier to understand.
- Point me to a portal that you believe is patient friendly, put on your flak jacket and give me 30 minutes to make you understand that the portal smells worse than pig effluent.
- Why would I be forced to go through all of the userID creation (I have somewhere around 250 of them in my Google profile) etc. just to give doctors access? Why can’t I tell the people at the radiology site that Drs A, D, V & Z can have access? I am extremely engaged in my health as a nearly 30 yr Type 1 Diabetic. But what you just described sounds like more PITA administration that I have ZERO interest in.
- You cannot force adoption, it comes to good products and causes bad ones to fail.
- I am committed to health (as opposed to healthcare) and I take an active approach to wellness. [ . . . ] Since my hospital-employed PCP implemented EPIC, my relationship with that office and my doctor has significantly degraded. The implementation of EHR and its patient portal caused me to disengage, not engage.
- Meaningful Use is the worst government policy since the Vietnam Conflict. Over 75% of doctors have stated that MU is a disaster and patients are waking up to this fact.
- EPIC and others have developed their EHR to generate revenue for the healthcare providers and they are forced to create patient portals due to regulations.
- Whatever use case you can think of, the patient MUST gain value in issuing a portal (I hate this 15 yr out of date term…) or you’re causing them pain and suffering just to cut administrative costs for the provider.
- We have to address “what is in it for me?” [when I comes to patient use]. The point is that barely nobody is engaged towards tools
- Give me a bad patient outcome and an EMR primarily designed to bill, that allows cut and paste, and populates differential diagnoses without requiring the provider to rule each out, and I will show you a lost med mal case.
- We are looking to technology to fix a human problem… taking their health for granted.
- Providers, use the portal to tell your patients how they can help you be most efficient. Have your EHR builders “put your heart in your letters” why this is a valuable resource, that you support it also.
- If the providers don’t trust it, neither will the patients, and then it [patient portal] truly is useless.
Take Aways?
No surprises here. When people in the business are honest about it, based upon my limited, informal sample, many just don’t buy into the patient engagement-Health IT hype.
Of the 70+ responses
- No one “believes” that health IT actually “creates or drives” engagement where it did not already exist.
- Many recognize that patient engagement occur between patients and their physicians – HIT is just useful medium for supporting that relationship.
- There are lots of problems with patient portals beginning with:Their purpose
- Who really benefits (clinician-patient-payer)
- Terms and conditions of use, e.g., legalese
- Relevance
- Usability
- Interoperability
- “Byzantine” Sign In and User ID Practices
- Some believe that portals actually caused them to “disengage” rather than engage
- How one “rolls out” their portal to patient and physicians is critical
The bottom line when it comes to portals I would offer the following advice:
- Be clear about why you are implementing a patient portal
- Involve patients (and clinicians) in the planning and development
- Enroll clinicians to introduce portal to their patients
- Be clear about what constitutes success, including how you will measure it