In Fact It’s Downright Disengaging…
Stop the presses! I now have access to my very own personalized patient portal courtesy of my personal physician. The big event occurred this last Tuesday. I have to admit I was a bit excited that my doctor was slowly merging onto the information super highway. Heck he even sprang recently for an out-of-the box EMR system which he is forever complaining about.
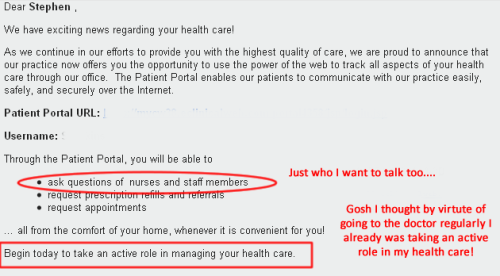
But my excitement was short lived. Very short lived in fact after reading the e-mail from E-Clinicalworks (the patient portal vendor) which I am sharing with you here.
Now I realize that my doctor works in a solo practice as part of a large IPA…not the Mayo Clinic. But this email…and presumably everything associated with this patient portal is…well…very amateurish and totally disengaging.
A couple of things immediately jumped out at me while reading this e-mail invitation to my patient portal.
The patient portal claims to offer me “the power of the web to track all aspect of my care through my doctor’s office.”That’s pretty powerful!
But I read on to discover that my physician’s concept of what I should have the “power” to do and what he thinks I should be able to do is very different. Why am I surprised…?
First there is no mention of any kind of access to my actual health information…and certainly not my “physician’s notes.”But that doesn’t mean I am willing to leave my doctor for someone who offers this capability.
Second…and perhaps most galling…is that I can’t actually communicate with my doctor via the portal. I can email his office staff…and maybe they will respond and maybe not. In the non-digital world they would get back to me at their own leisure.
Third, I can’t actually do anything on the portal (as configured by my doctor) other than request that the surly office staff intervene with the doctor to refill my prescriptions. Asking is certainly different than doing in my book. How the heck is this supposed to make me feel engaged?
Finally the email presumes to tell me that up until today my physician apparently does not think that I have been taking an active role in my own health care. Let me get this right…I am 100% compliant with my medications, exercise, see my doctor regularly and am in good shape…yet I am not actively involved in my own health. Come on now.
In its favor…the email was personalized – it got my first name right. It never did mention my doctor’s name or his office address.
Upon getting this email from my doctor I was immediately reminded of a quote from a recent Dave Chase Forbes article about the value of physician-patient communications in which he said this about patient portals:
“The smart healthcare providers realize simplistic patient portals, however, won’t get the job done. Simple patient portals are like a muddy puddle of water in the Sahara Desert — a big improvement but far from ideal.
Kudos to physicians everywhere that are trying… But please recognize that your patients are not simpletons and that they are already engaged in their health at least from their perspective. For portals like this to be successful – (meaning that patients actually use them more than once) – they need to offer real value (from the patient’s perspective), they need to be relevant to patients (not you or your staff) and they need to respect my intelligence.
Take Aways
Most patients are already engaged in their own health care. The biggest challenge for providers today is not so much engaging patients but rather to avoid disengaging them.
I realize that my experience offers but one example of a patient portal gone wrong. If you have samples of patient portal experiences you would like to share e-mail me at stwilkins at gmail.com.